The main obstacle to getting a better electronic health care record off the ground is the following. Hospitals (or large primary care organizations, for that matter) generally do not buy anything but complete systems with wall-to-wall coverage of functionality, which in turn leads to major upheavals at every system change and generally an almost total loss of all information that was kept in the legacy systems. Even if the legacy information is kept in some form, it is usually so hard to retrieve as to make it, for all practical purpose, gone.
The only way forward is to break this vicious circle. Hospital systems have grown too large to be built as monolithic products by single companies and in practice we see each generation of medical records system becoming much richer in diversity of functionality and much poorer in execution of the individual functions, including poor analysis and implementation, and with ever increasing bug counts and dangerous failures.
(A very fundamental problem is that all these systems implement a medical records model that was never intended for this use. Medical records were developed to serve as a memory aid to a family physician and was never structured to help in managing disease. I wrote a little “history” of medical records to illustrate what I mean by this and what went wrong when this one-physician system was scaled up.)
In order to get out of this situation, it’s absolutely necessary to create a market where smaller, interacting systems can be produced and marketed. A number of efforts are being done, mainly as European projects (e.g. OpenEHR), but as often happens, these projects are large and slow to result in actual products, but they do contain a number of interesting results that we do intend to reuse. The participation of customer organisations show that interest is high in this type of open development. From my informal contacts, it is clear that most hospitals have knowledgeable personnel eager to test and run smaller, open systems that would help them solve otherwise intractable problems, but the monolithic systems they have installed won’t let them do this on their own.
In other words, to enable us to develop smaller systems that are more suitable for their purpose than the huge compromise systems of today, we must develop an open market, a market built on public and open standards, and to a large degree on open software. The standards need to be of the “American variety”, that is selected from actually working implementations and not, as is more common in Europe, designed by committee.
The only realistic way of getting new systems into hospitals is not to replace existing systems, but to complement them. To be able to do that, the new systems must connect to existing systems and provide an added value. The iotaMed system we’re defining does just that.
Our business idea is to create a market for open systems and system additions to existing monolithic installations, show that it is possible and how it is to be done, and then sell into that new market both products and services to implement the iotaMed overlay.
It is clear that we need cooperation from other smaller actors to create and maintain a productive market of modules, and to do that we cannot keep neither the standards nor the products proprietary. If you want to go the proprietary route, you must be as large as the current players and we are not, and do not desire to be, since we would then produce the same inferior products and compete in a market in which we could not win.
The last number of years have shown that it is not necessary to have proprietary products and standards to achieve business success in the software arena. Companies such as Red Hat and MySQL have profited greatly from creating and maintaining an open market for their systems, giving away their products and standards for free (with “enterprise” exceptions), while having a very respectable income from support and consultancy.
We propose basically the same business idea as them, namely build a market of open systems and standards, then sell into that market support and advisory functions, plus a few signature products such as the iPad implementation of the user interface and communication systems.
As to the argument we often get that this change is only for the younger generation and that the older generation will resist it, I have this to say. First, younger doctors aren’t that hot, either, simply because they usually get their habits from their supervisors. It’s amazingly rare to find even 25 year olds daring to type in the medical records; they all dictate in Sweden. On the other hand and as far as I know, all doctors type for themselves in Norway, irrespective of age.
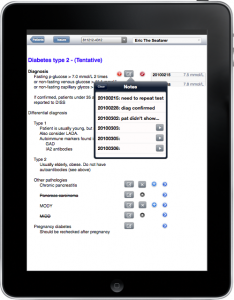
Secondly, all doctors are subject to change, if they want to or not. All doctors now must read the electronic healthcare record, which implies hugely increasing amounts of data to wade through and an uncomfortable way of making sense of it. Adding an organizing overlay such as iotaMed would provide doctors a huge relief from the drawbacks of automation and information overload gone wild, making it easier for them all, young and old alike.
Comparing iotaMed to other dissimilar initiatives such as the Microsoft and Google initiatives, and the Swedish NPÖ, we see they all have at least one problem in common and that is that all these systems are created with the idea that more information is good, but that is not necessarily so. Too much prose without structure is worse than useless and even the most important data drowns in the flood. None of these projects have shown that any priority is given to the actual structuring of information according to planning and modern clinical principles. They’re simply firehoses of information. It seems as if nobody has ever studied the psychological impact on the user of these systems. Why not, is a major mystery to me.
Another problem they do not adress is how to connect evidence based medicine to clinical practice. Coincidentally, these two problems are not only the major obstacles to efficient healthcare, but also the two problems iotaMed sets out to solve.
I’ve tried out my ideas with pen and paper on a few GPs in all age groups. There was no clear difference in how quickly the doctor saw the advantages and the point of it. Rather, the older doctors seemed quicker to pick it up, since they have a more acute feeling of losing contact with scientific advances and they also more acutely feel how much control they are losing over the patient history, which used to be much more tractable a number of years back. Younger doctors don’t yet see the downward slope as clearly.